Hospice is specialized care for people with a serious illness who prefer comfort and quality of life. Hospice eligibility is a clinical and regulatory decision. Patient readiness is a human decision that involves insight, preferences, and caregiver capacity.
Separating eligibility from readiness helps Clinicians refer earlier, document with confidence, and choose the right level of care for patients in Fulton County and Alpharetta, Georgia. This guide explains the difference in plain terms and gives you practical tools you can use today.
Why This Distinction Matters for Your Patients

Families in Metro Atlanta often meet criteria for hospice long before they feel prepared to enroll. You can acknowledge both truths at once. You determine that a patient is eligible based on prognosis and objective indicators. You support readiness through conversations, caregiver assessments, and practical planning. Doing both helps your patients avoid crisis admissions in Fulton County hospitals and allows more time at home in Alpharetta and nearby communities.
What Hospice Eligibility Means
Eligibility answers a narrow question. Can this patient receive the hospice benefit now based on a reasonable expectation of six months or less if the disease runs its normal course, supported by documentation and physician certification.
Document the following every time:
- Primary diagnosis and trajectory that support a six-month prognosis using objective markers aligned with accepted indicators for the condition.
- Functional decline using PPS or KPS, recent weight loss, decreased oral intake, falls, infections, or emergency visits.
- Related comorbidities that accelerate decline and affect symptom control.
- Two-step certification by the attending or hospice physician, followed by an individualized plan of care.
If your patient resides in Alpharetta or elsewhere in Fulton County, note living situation, travel burden, and access to caregivers. This supports level-of-care planning once the patient elects hospice.
Patient Readiness Meaning
Readiness is broader. It reflects whether the patient and care network understand the illness, agree with comfort-focused goals, and can safely participate in hospice care today.
Readiness points to evaluate:
- Prognostic understanding and goals: Does the patient understand the likely course and prefer comfort, time at home, and less burdensome care.
- Caregiver capacity: Who provides day-to-day help in the home, who is backup, and what skills or education are needed.
- Symptom burden and safety: Are pain, dyspnea, agitation, or delirium manageable at home, or is a short general inpatient stay appropriate to stabilize symptoms.
- Cultural and spiritual preferences: What rituals, language needs, or faith traditions should guide the plan.
Practical Steps for Fulton County Clinicians
- Screen for Likely Eligibility Early. Review PPS or KPS trends, unplanned hospital or ED use, infections, falls, and weight loss. Capture objective data in your note. If uncertain, request an informational consult to confirm criteria and fill gaps in documentation.
- Start Readiness Conversations Before a Crisis.
Use simple, direct language and check understanding.
- “Given how your illness is changing, would focusing on comfort and time at home fit what matters most to you.”
- “Here is how hospice works in our area, including medications, equipment, and 24-hour support.”
Offer a no-obligation informational visit. Many Fulton County families appreciate meeting the team in the home in Alpharetta or by phone first. To help families take the next step, read our guide, How to Start Hospice Care in Alpharetta, which explains who to call, what to prepare, and what to expect.
- Assess Caregiver Capacity and Home Resources. Identify the primary and backup caregivers, transportation, work schedules, and home layout. Screen for burden and training needs, such as medication administration, oxygen use, or safe transfers. When capacity is limited, plan for short-term general inpatient care or continuous home care to stabilize symptoms, then transition to routine home care.
- Match the Initial Levels of Care on Day One. Choose the least intensive level that safely meets needs, with clear triggers to escalate.
- Routine Home Care: Symptoms are controlled with intermittent nursing, social work, chaplaincy, and aide support.
- Continuous Home Care: Time-limited skilled nursing for acute symptom crises at home.
- General Inpatient Care: Facility-based care for uncontrolled symptoms that cannot be managed at home.
- Inpatient Respite: Short stay to support caregiver relief.
Learn more about the four Medicare-covered levels of hospice care and our Transitional Care pathway.
- Document Eligibility vs Readiness.
- Eligibility section: prognosis rationale tied to objective markers, functional scales, comorbidities, and why a six-month expectancy is reasonable.
- Readiness section: goals of care, informed consent elements, caregiver assessment, education provided, preferred location of care, and the initial level of care with a safety plan.
Conversation Prompts You Can Use Immediately
- “If we could make your days more comfortable at home in Alpharetta, what would that look like?”
- “Who is with you most days, who helps at night, and who can fill in when that person works.”
- “If your pain worsens, would a short stay for intensive symptom management feel acceptable, then a return home when comfortable.”
Quick Tools for Objective and Compassionate Practice
- PPS or KPS: Record current scores and trends, add a brief interpretation linked to the prognosis statement.
- Diagnosis quick checks: Keep short references for dementia, heart failure, COPD, cancer, stroke, or ALS that reflect widely used indicators.
- Caregiver readiness checklist: Primary and backup names, tasks they can do now, training needed, barriers, and a plan for after-hours support.
- Plan-of-care starter set: Pain and dyspnea plans, equipment list, after-hours escalation instructions, and criteria for CHC or GIP.
Common Pitfalls in Metro Atlanta and How to Avoid Them
- Waiting for full readiness before referring: Refer when clinical criteria are met. Use informational visits to build readiness while you continue disease-directed care.
- Vague prognosis notes: Tie functional scales and recent events to the six-month expectancy. Quote objective data.
- Unclear starting level of care: Justify routine home care versus CHC or GIP based on symptoms and caregiver capacity. State triggers for escalation.
- Missed caregiver education: Record who attended, what you taught, teach-back confirmation, and key preferences.
How Golden Rule Hospice Supports Patients in Alpharetta
You can refer for an informational visit or formal admission. Our team provides:
- Same-day or next-day informational visits in Fulton County, including Alpharetta and neighboring communities, to build insight and readiness.
- Eligibility review with clear, indicator-based documentation, including PPS or KPS and disease-specific markers.
- Matching to the correct Medicare-covered level of care, with a clear path to escalate if symptoms change.
- An exclusive Transitional Care pathway that eases patients and families into hospice when timing and preferences call for a gentler start.
Discuss a Case with Us in Alpharetta
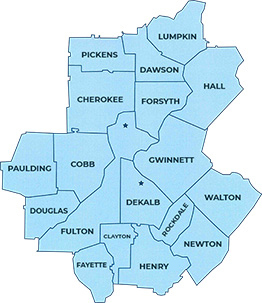
Call (470) 395-6567 to inquire about a case or request an informational visit now. A hospice nurse can speak with you or the family, review indicators, and suggest the safest starting level of care. Golden Rule Hospice supports patients and families throughout Fulton County, including Alpharetta, Roswell, Sandy Springs, Johns Creek, and surrounding communities.