You want predictable, goal-concordant care for patients with advancing illness without losing continuity or overwhelming your clinic after hours. A strong hospice partnership makes that possible.
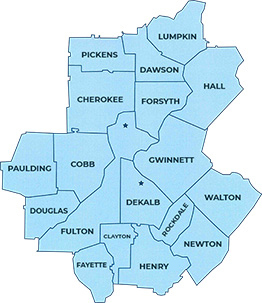
This guide outlines how collaboration works in Alpharetta, North Fulton, and surrounding Metro Atlanta communities, so you can refer confidently and stay connected to your patients.
How Early Hospice Referral by Physician Helps

Early hospice involvement supports symptom control, reduces unplanned utilization, and gives families a clear plan for nights and weekends. For your practice, it means fewer crisis calls, less moral distress, and more time for the visits only you can deliver.
Our team at Golden Rule Hospice functions as an extension of yours: reinforcing your goals, updating you promptly, and managing after-hours escalations with a clear protocol.
Shared-Care Model: Physicians Stay in the Loop
Hospice is not a handoff; it is shared care.
- Your role remains central. You can continue as attending or designate the hospice physician; either way, we loop you in on changes, orders, and goals-of-care updates.
- Communication you can count on. Expect concise progress notes, medication changes, and significant-event updates. We align documentation with your preferences (fax, secure email, or EMR bridge where available).
- Care plan transparency. You receive the initial plan of care and subsequent updates at each review cycle, plus immediate contact for any acute change.
First 72 Hours: What to Expect After You Refer
A clear early rhythm builds trust with your patients and your team.
- Day 0-1: Intake and Stabilization
- We confirm eligibility, review meds, capture goals, and begin symptom relief immediately.
- We arrange equipment (e.g., hospital bed, oxygen) and deliver a comfort-medication kit when appropriate.
- You receive a brief admission summary with baseline symptoms and first-line plans.
- We confirm eligibility, review meds, capture goals, and begin symptom relief immediately.
- Day 2-3: Team Alignment and Routines
- Nurse, social worker, aide, and chaplain introduce roles.
- Aide schedule begins for personal care support; caregiver education starts (e.g., safe mobility, breakthrough symptom plans).
- We send you medication reconciliation and any request for order clarifications.
- Nurse, social worker, aide, and chaplain introduce roles.
- Day 3-5: Fine-Tuning and Contingency Planning
- We adjust medications to balance alertness and comfort.
- We provide a written “what-if” guide for caregivers (pain flares, dyspnea, anxiety, fever).
- You receive a concise progress update and next review date.
- We adjust medications to balance alertness and comfort.
When to Refer to Hospice in Fulton County
Consider a hospice consult when you observe one or more of the following:
- Two or more ED visits or hospitalizations in the last 90 days for the same progressive condition.
- Functional decline: more time in bed or chair, new dependence in two or more ADLs.
- Weight loss, dysphagia, or recurrent infections despite appropriate disease-directed care.
- A patient or family prioritizing time at home and comfort over additional hospital-based interventions.
When in doubt, refer for information only. We can track, support, and coordinate with you until eligibility is clear. Discover eligibility and patient readiness when it comes to hospice in our guide: Hospice Eligibility vs Patient Readiness.
Eligibility Triggers by Condition
These prompts help you identify patients who benefit from hospice evaluation. Use clinical judgment; call us if you’re unsure, we’ll help you think it through.
- Dementia: FAST stage 7; weight loss, recurrent infections, limited verbal ability, total dependence in ADLs.
- Heart disease (CHF, ischemic): Frequent hospitalizations or ED visits, refractory symptoms at rest, hypotension limiting guideline-directed therapy, progressive renal dysfunction.
- Pulmonary disease (COPD, ILD): Dyspnea at rest or minimal exertion despite optimal therapy, unintentional weight loss, home oxygen escalation, frequent steroid bursts or infections.
- Cancer: Progressive, treatment-refractory disease; ECOG 3–4; declining functional status; symptom burden out of proportion to benefit from further disease-directed therapy.
- Neurologic disease (ALS, Parkinson’s, stroke): Progressive dysphagia, recurrent aspiration or infections, weight loss, inability to perform ADLs without assistance.
If you’re on the fence, a no-obligation information visit can help set expectations while we track function and symptoms over time.
The Five Levels of Support We Provide
Medicare defines four levels of hospice care; we provide all four and add Transitional Care to smooth starts and changes.
- Routine home care: Most patients, regular RN, aide, social work, chaplain visits at home or in a senior community.
- Continuous home care: Short-term, intensive nursing at home for symptom crises to avoid the hospital when appropriate.
- General inpatient care: Short-term inpatient management if symptoms cannot be controlled at home.
- Respite care: Brief inpatient stays to give caregivers relief.
- Transitional Care (our program): Additional touchpoints and coordination during admission and status changes to prevent gaps.
These flexible levels let us match intensity to need, then step down as stability returns. (Medicare’s four levels are standardized nationally)
What We Handle vs. What You Keep
We Handle:
- 24/7 triage and urgent symptom visits.
- Comfort-focused medications related to the terminal diagnosis (procurement, titration, teaching).
- DME delivery and setup (hospital bed, oxygen, commode, wheelchair).
- Caregiver education, psychosocial and spiritual support, and bereavement services.
- Coordination with facilities (assisted living, memory care, SNF) and home health where applicable.
You Keep:
- Oversight if you choose to remain attending.
- Non-hospice-related conditions and scripts not tied to the terminal diagnosis, as appropriate.
- Specialty input on disease-specific nuances; we welcome your preferences for thresholds and algorithms.
Documentation Checklist to Speed Referrals
Having these on hand often prevents delays:
- Most recent H&P and problem list.
- Last two months of progress notes (helpful for documenting decline).
- Pertinent labs/imaging that inform prognosis or symptom burden.
- Medication list with recent changes and intolerances.
- Contact info for POA/healthcare proxy and preferred pharmacy.
- Any advanced directives or POLST forms, if available.
Not sure whether the chart tells the full story? A quick call to (470) 395-6567 or online visit gets you a same-day consult to review red flags and functional decline.
After-Hours, Weekends, and Holidays: No Loose Ends
Nighttime dyspnea, agitation, fever, and uncontrolled pain are predictable stress points. Our protocol includes:
- 24/7 RN triage with nurse-to-nurse escalation criteria.
- In-person crisis visits when home measures are insufficient.
- Comfort kit guidance and on-call pharmacy coordination.
- Clear guidance for when inpatient care is the safest next step.
Your on-call burden is lighter, and your patients avoid defaulting to the ED for symptom spikes.
Practical Ways We Reduce Friction for Your Clinic
- Single-call referral. One number for consults and admissions: (470) 395-6567.
- Fast equipment turnaround. Local vendors and established pathways across North Fulton speed delivery.
- Concise updates. Bullet summaries, med changes highlighted, next steps specified.
- Proactive caregiver teaching. We script what to do for the top five likely symptom changes to prevent panic calls to your office.
- Community ties. Familiarity with Alpharetta hospitals, senior communities, and faith partners helps us solve problems quickly.
How to Refer
- Call (470) 395-6567 for a curbside consult or direct admission request.
- Send recent notes, med list, and contacts via secure fax or EMR.
- Set the expectation with the patient/family using one sentence: “The hospice nurse will visit within 24 hours to start comfort measures and set up equipment.”
- We will confirm with you once admitted and send the initial plan of care.
Coverage and Costs: What Patients Need to Hear
Medicare’s hospice benefit covers interdisciplinary care, medications and equipment related to the terminal diagnosis, and 24/7 support. There may be small coinsurance for respite care. Patients can revoke hospice if goals change and may be re-certified if they remain eligible. Sharing these points reduces fear and helps families say “yes” sooner.
Get Local Hospice Partnership Today
Partner with a trusted hospice provider in Alpharetta for timely referrals and responsive shared care. Call (470) 395-6567 today so your patients have comfort, clarity, and continuity, and your practice has a reliable partner after hours.
We serve patients where they live: homes, assisted living, and memory care communities across Alpharetta, North Fulton, and nearby Metro Atlanta counties. You’ll get a team that treats your patients and staff like neighbors, keeps you informed, and shows up when it matters.